Post by Nadica (She/Her) on Aug 26, 2024 20:34:24 GMT
The COVID-19 thrombus: distinguishing pathological, mechanistic, and phenotypic features and management - Published Aug 23, 2024
Abstract
A heightened risk for thrombosis is a hallmark of COVID-19. Expansive clinical experience and medical literature have characterized small (micro) and large (macro) vessel involvement of the venous and arterial circulatory systems. Most events occur in patients with serious or critical illness in the hyperacute (first 1–2 weeks) or acute phases (2–4 weeks) of SARS-CoV-2 infection. However, thrombosis involving the venous, arterial, and microcirculatory systems has been reported in the subacute (4–8 weeks), convalescent (> 8–12 weeks) and chronic phases (> 12 weeks) among patients with mild-to-moderate illness. The purpose of the current focused review is to highlight the distinguishing clinical features, pathological components, and potential mechanisms of venous, arterial, and microvascular thrombosis in patients with COVID-19. The overarching objective is to better understand the proclivity for thrombosis, laying a solid foundation for screening and surveillance modalities, preventive strategies, and optimal patient management.
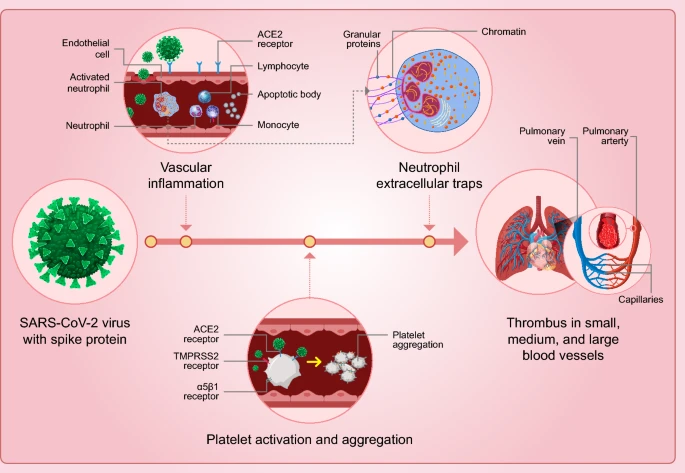
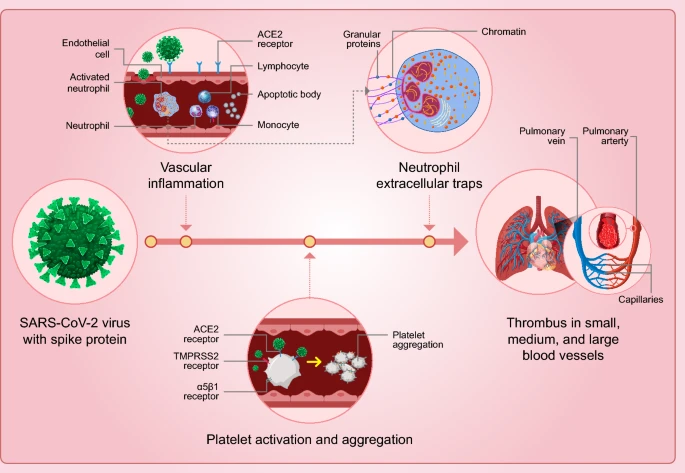
Graphical abstract
Thrombosis involving the arterial, venous, and microvascular circulatory systems is a hallmark of COVID-19 contributing to organ injury, morbidity, and mortality. The COVID-19 thrombus has unique and distinct characteristics. Among them are a highly inflammatory signature on a foundation of endothelial cell inflammation and neutrophil extracellular traps (NETs). While the SARS-CoV-2 virus and resulting host immunoinflammatory response to this pathogen provide an underpinning for vascular events, the virus spike protein is necessary and likely sufficient for acute, subacute, and potentially in a latent form harbored in adipocytes, vascular endothelial cells, and circulating monocytes potentially contributing to post-infectious atherothrombotic phenotypes.
Abstract
A heightened risk for thrombosis is a hallmark of COVID-19. Expansive clinical experience and medical literature have characterized small (micro) and large (macro) vessel involvement of the venous and arterial circulatory systems. Most events occur in patients with serious or critical illness in the hyperacute (first 1–2 weeks) or acute phases (2–4 weeks) of SARS-CoV-2 infection. However, thrombosis involving the venous, arterial, and microcirculatory systems has been reported in the subacute (4–8 weeks), convalescent (> 8–12 weeks) and chronic phases (> 12 weeks) among patients with mild-to-moderate illness. The purpose of the current focused review is to highlight the distinguishing clinical features, pathological components, and potential mechanisms of venous, arterial, and microvascular thrombosis in patients with COVID-19. The overarching objective is to better understand the proclivity for thrombosis, laying a solid foundation for screening and surveillance modalities, preventive strategies, and optimal patient management.
Graphical abstract
Thrombosis involving the arterial, venous, and microvascular circulatory systems is a hallmark of COVID-19 contributing to organ injury, morbidity, and mortality. The COVID-19 thrombus has unique and distinct characteristics. Among them are a highly inflammatory signature on a foundation of endothelial cell inflammation and neutrophil extracellular traps (NETs). While the SARS-CoV-2 virus and resulting host immunoinflammatory response to this pathogen provide an underpinning for vascular events, the virus spike protein is necessary and likely sufficient for acute, subacute, and potentially in a latent form harbored in adipocytes, vascular endothelial cells, and circulating monocytes potentially contributing to post-infectious atherothrombotic phenotypes.